Hypoxia, the insufficient supply of oxygen, is something that almost every oxygen using organism since the dawn of life encountered in its lifetime. Ever woke up to a numb arm at night? That is hypoxia. Ever grew a little? The hypoxia in the new tissue directs your blood vessels to grow in order to maintain proper supply. Ever held your breath? That also caused hypoxia.

Although our lives depend on oxygen, our conscious selves surprisingly don’t have reliable ways to sense when our bodies go to hypoxic states. When we hold our breaths, the rapid buildup of CO2 in our body leads to all the unpleasant feelings and reflexes that force us to breathe again. But if the levels of oxygen in the air we breathe drop rapidly for whatever reason, the symptoms of hypoxia may go unrecognized by an untrained person. One of the reasons for this is that the brain is the first organ to suffer from lack of oxygen, which usually leads to loss of proper judgement.
However, our cells sense and respond to hypoxia practically immediately, whether it comes from changes within the body or lack of oxygen in the air. Depending on which tissues are sensing the lack of oxygen, the response can be very varied, but there are some general commonalities. It is useful to look at adaptations to hypoxia from two points of view – at the cellular level and systemically.
On the cellular level, cells experience a range of adaptive responses and may undergo various changes that can affect their function and survival. They can decrease their consumption of energy and alter their metabolism until oxygen levels are restored. Hypoxia is often associated with activation of autophagy, the process of destruction of unnecessary or damaged components of the cell. Autophagy helps cells to overcome hypoxic challenges by capturing and breaking down cellular components and recycling the nutrients to generate new energy and cellular building blocks. All these changes together promote cell survival and adaptation in hypoxic conditions.
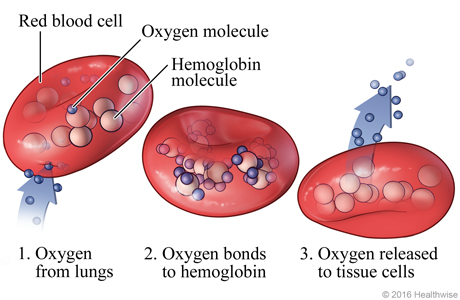
On the systemic level, hypoxia is first sensed by special chemoreceptor centres in our aortas. Under normal conditions, these centres do not affect our breathing. When oxygen drops significantly, their activity dramatically increases and they override the breathing regulation in our brain despite the CO2 levels in our blood drops. Furthermore, cardiac output increases to pump more blood into our tissues and in most tissues the blood vessels dilate to better supply the tissue with oxygen. If hypoxia lasts longer than a few moments, our bodies take further actions to adapt. Our kidneys start producing erythropoietin, a circulating hormone which stimulates the production of red blood cells and hemoglobin, the main transport vessels of oxygen in our organism. Furthermore, erythropoietin stimulates angiogenesis, the growth of new blood vessels so that our tissues are well supplied with oxygen.
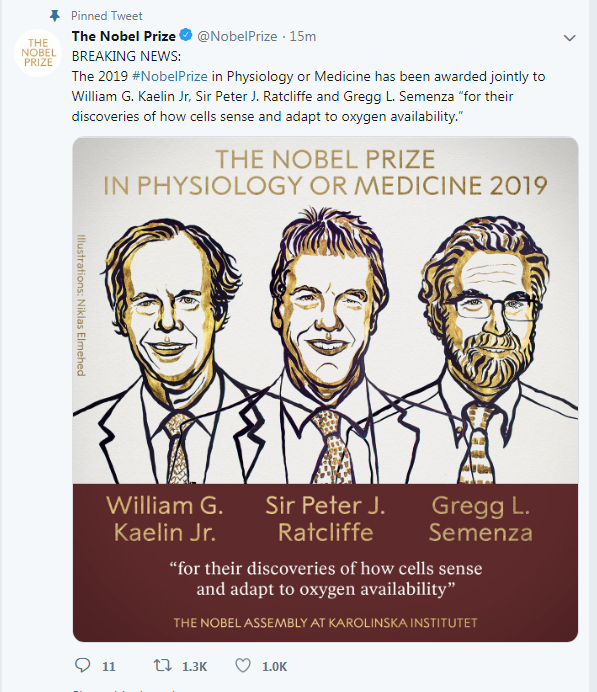
How hypoxia is regulated on the molecular level was not understood until the discovery of Hypoxia-inducible factors (HIFs) in 1995. This scientific breakthrough was honored with the 2019 Nobel Prize in Physiology and Medicine awarded jointly to William G. Kaelin Jr, Sir Peter J. Ratcliffe, and Gregg L. Semenza “for their discoveries of how cells sense and adapt to oxygen availability”.